Congenital Glaucoma
👶 Congenital Glaucoma (Pediatric Glaucoma)
Also known as Primary Congenital Glaucoma (PCG) or Infantile Glaucoma
🧠 Definition
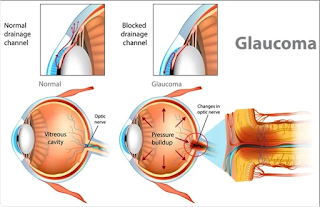
Congenital glaucoma is a rare condition present at birth or within the first few years of life, caused by abnormal development of the eye’s aqueous outflow system, especially the trabecular meshwork and anterior chamber angle, leading to increased intraocular pressure (IOP).
🔍 Types of Congenital Glaucoma
-
Primary Congenital Glaucoma
-
Isolated developmental abnormality
-
Bilateral in 70–80% of cases
-
Most common form of glaucoma in infancy
-
-
Secondary Congenital Glaucoma
-
Associated with ocular or systemic conditions like:
-
Axenfeld-Rieger syndrome
-
Peter’s anomaly
-
Sturge-Weber syndrome
-
Aniridia
-
-
-
Infantile and Juvenile Glaucoma
-
Infantile: onset after 1 month but before 3 years
-
Juvenile: onset after age 3 to early adulthood
-
🧬 Etiology & Pathogenesis
-
Developmental anomaly of the trabecular meshwork and anterior chamber angle obstructs aqueous humor outflow.
-
Leads to elevated IOP, stretching the eye structures (as the infantile eye is still elastic), and eventually damaging the optic nerve.
👁️ Clinical Features (Classic Triad)
| Symptom | Explanation |
|---|---|
| Epiphora (Tearing) | Due to corneal irritation from high IOP |
| Photophobia | Light sensitivity caused by corneal edema |
| Blepharospasm | Involuntary tight closure of eyelids |
Additional signs:
-
Buphthalmos: Enlargement of the eyeball
-
Corneal clouding due to edema
-
Haab’s striae: Horizontal breaks in Descemet’s membrane
-
Enlarged corneal diameter (>12 mm)
-
Optic disc cupping
-
Elevated IOP (>21 mmHg)
🩺 Diagnosis
-
Examination under anesthesia (EUA)
-
Accurate IOP measurement
-
Corneal diameter
-
Gonioscopy (angle evaluation)
-
Fundus examination (optic disc)
-
-
Tonometry
-
Use pediatric-friendly instruments (e.g., Perkins, Tono-Pen)
-
-
Ultrasound Biomicroscopy (UBM) or AS-OCT
-
Evaluates anterior segment structures
-
💊 Management
1. Surgical Treatment (Mainstay)
| Procedure | Indication |
|---|---|
| Goniotomy | First-line if cornea is clear |
| Trabeculotomy | If cornea is cloudy |
| Combined Trabeculotomy-Trabeculectomy | For advanced or resistant cases |
| Glaucoma Drainage Devices | For failed previous surgeries |
| Cycloablation (Cyclophotocoagulation) | As a last resort |
2. Medical Treatment (Supportive/Pre-op)
-
Used temporarily to control IOP before surgery
-
Beta-blockers (e.g., Timolol) – caution in infants
-
Carbonic anhydrase inhibitors (e.g., Acetazolamide)
-
Prostaglandin analogs – variable effectiveness
-
Miotics (Pilocarpine) – limited role
🔄 Follow-Up & Prognosis
-
Regular monitoring of IOP, optic nerve, visual acuity, and eye growth
-
Lifelong follow-up needed
-
Prognosis depends on age at diagnosis, timing of surgery, and degree of optic nerve damage
⚠️ Complications if Untreated
-
Permanent vision loss / blindness
-
Amblyopia
-
Strabismus
-
Corneal scarring
-
Photophobia & cosmetic disfigurement
📝 Summary Table
| Feature | Details |
|---|---|
| Onset | Birth to 3 years |
| Triad | Epiphora, Photophobia, Blepharospasm |
| Eye enlargement | Buphthalmos |
| Diagnosis | EUA, tonometry, gonioscopy |
| Treatment | Surgical (goniotomy/trabeculotomy) |
| Medical Rx | Temporarily lowers IOP pre-surgery |
| Prognosis | Better with early detection & treatment |
Comments
Post a Comment