Open-Angle Glaucoma
👁️🗨️ Open-Angle Glaucoma (OAG)
Also known as Primary Open-Angle Glaucoma (POAG) — the most common type of glaucoma worldwide.
🧠 Definition
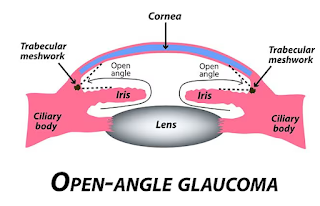
Open-angle glaucoma is a chronic, progressive optic neuropathy caused by increased resistance to aqueous outflow through the trabecular meshwork, leading to elevated intraocular pressure (IOP) and gradual damage to the optic nerve — even though the anterior chamber angle remains anatomically open.
🔬 Pathophysiology
-
Aqueous humor flows from the ciliary body → posterior chamber → pupil → anterior chamber → drains via trabecular meshwork → Schlemm’s canal → episcleral veins.
-
In OAG:
-
The drainage system becomes inefficient over time.
-
Intraocular pressure rises, damaging the retinal ganglion cells and optic nerve fibers, particularly in the superior and inferior poles, leading to cupping and visual field loss.
-
-
Despite the name, the angle remains open on gonioscopy.
📊 Epidemiology
-
Most common in individuals >40 years
-
Leading cause of irreversible blindness worldwide
-
More prevalent in:
-
African descent
-
Family history of glaucoma
-
Diabetics
-
Myopes (nearsighted)
-
🔍 Clinical Features
🐢 Silent Progression (Until late stages)
| Early signs | Late signs |
|---|---|
| Usually asymptomatic | Peripheral vision loss (tunnel vision) |
| Slight eye discomfort (rare) | Poor night vision |
| No redness or pain | Eventual central vision loss |
🩺 Diagnosis
-
Tonometry
-
Measures IOP (usually >21 mmHg in POAG)
-
Note: Some POAG patients may have normal IOP (Normal-Tension Glaucoma)
-
-
Gonioscopy
-
Confirms open angle in anterior chamber
-
-
Ophthalmoscopy / Fundus Examination
-
Increased cup-to-disc ratio (>0.6)
-
Thinning of neuroretinal rim
-
Optic disc cupping
-
-
Visual Field Testing (Perimetry)
-
Detects peripheral field defects early
-
Arcuate scotomas, nasal step, paracentral defects
-
-
OCT (Optical Coherence Tomography)
-
Measures retinal nerve fiber layer thickness and ganglion cell layer loss
-
-
Pachymetry
-
Measures central corneal thickness (affects accuracy of IOP readings)
-
💊 Treatment
🎯 Goal: Lower IOP to prevent progression
1. Medical Therapy (First-line)
| Drug Class | Examples | Action |
|---|---|---|
| Prostaglandin analogs | Latanoprost, Travoprost | ↑ Uveoscleral outflow |
| Beta-blockers | Timolol, Betaxolol | ↓ Aqueous production |
| Alpha-agonists | Brimonidine | ↓ Production & ↑ Outflow |
| Carbonic anhydrase inhibitors | Dorzolamide, Acetazolamide | ↓ Production |
| Rho kinase inhibitors | Netarsudil | ↑ Trabecular outflow |
2. Laser Therapy
-
Laser Trabeculoplasty
-
Argon (ALT) or Selective (SLT)
-
Enhances trabecular outflow
-
Can be primary or adjunct therapy
-
3. Surgical Therapy
-
Trabeculectomy – Creates alternative drainage route
-
Drainage implants (e.g., Ahmed valve)
-
Minimally Invasive Glaucoma Surgeries (MIGS) – Safer, for mild/moderate cases
🔁 Follow-Up
-
Lifelong monitoring of:
-
IOP
-
Optic nerve status
-
Visual fields
-
Adherence to medication
-
-
Regular visits every 3–6 months
⚠️ Complications
-
Irreversible blindness if untreated
-
Depression and reduced quality of life due to vision loss
📌 Quick Facts
| Feature | Open-Angle Glaucoma |
|---|---|
| Angle status | Open |
| Onset | Insidious, chronic |
| Symptoms | None early; tunnel vision late |
| Pain/redness | Absent |
| IOP | Often elevated (>21 mmHg) |
| Emergency | No |
🧠 Normal-Tension Glaucoma (NTG)
-
A subtype of OAG with normal IOP (<21 mmHg)
-
Likely due to vascular dysregulation or optic nerve susceptibility
-
Risk factors: Low BP, sleep apnea, migraine
-
Managed similarly — goal is to lower IOP even further
Comments
Post a Comment